Decisions, Decisions
Universal healthcare can make decisions based on cost-benefit analysis; does it work for patients?
Last week, I wrote about a new drug intended to treat Alzheimer’s disease. Aduhelm was approved by the Food and Drug Administration (FDA) but very few neurologists or health systems are administering it because they believe it has limited benefit and significant risks. Additionally, Aduhelm costs about $30,000 per year per patient. In the article I discussed the idea that we are going to have to start adding economics to the drug approval process. For example, we will need to ask question such as: should Aduhelm be approved if it costs so much and has limited benefit?
Today, I want to examine the other side of the coin. What if there was a drug that had significant, even lifesaving, benefits that costs $300,000 per year? Should that drug be covered by a program like Medicare and what would happen if it wasn’t?
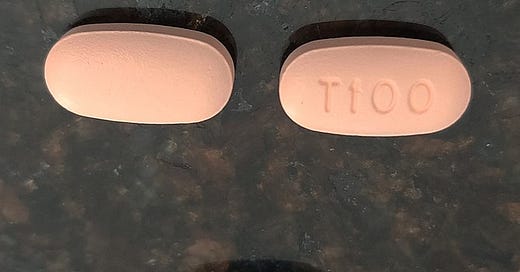
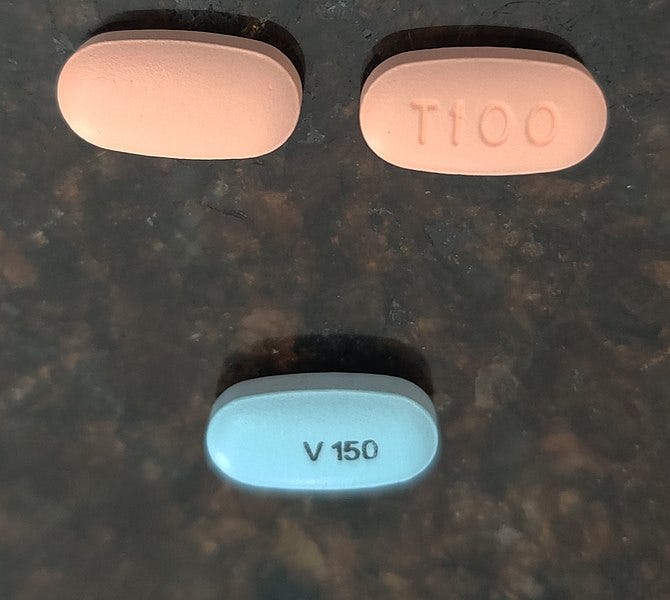
There may be a drug such as this. Trikafta is a drug (or rather a combination of three drugs) that is used to treat cystic fibrosis (CF). This treatment protocol has significant benefits for those suffering from CF and can be lifesaving. It does also cost $300,000 per year per patient.
Trikafta was approved for use in the United States in 2019. Many physicians and patients call Trikafta a game changer because it is dramatically improves the quality of life and extends the life of patients with CF. The drug was later approved in the United Kingdom in 2020 and in other parts of Europe over the last two years. This is good news.
In Australia, however, Trikafta was not approved until early 2021 and questions are being raised as to why it took the UK, Australia, and others so long to approve the drug. The simple answer is that they had to determine it was worth it.
What these countries have in common is their universal healthcare programs. The UK has the National Health Service (or NHS) and Australia has a system they call Medicare. These countries had to determine if the $300,000 price tag was worth it to approve and cover a drug in their healthcare systems. At the end of 2020, only twelve percent of CF patients around the world had access to Trikafta; even now there are areas that still do not have access to this game changing drug.
I want to be clear that this article is not an attack on universal healthcare nor is it an endorsement of the healthcare system we have in the US. Rather, I want to pint out that things are not as simple as we would like them to be. Universal healthcare is not a magic bullet. Like medications, universal healthcare can have harmful side effects.
For example, if you were a CF patient in Australia, you would know that one of those side effects is that you could not get a drug that you could get if you were in the United States and had health insurance. If you are an uninsured patient in the US, then you know the side effects of the high costs that you must pay directly for without universal healthcare.
As I said last week, I want to draw attention to these issues because they are things that we need to deal with. Of course, they are not easy and do not have easy answers. In the end, we will probably have to come up with some sort of compromise or balancing act.
How do we cover the most people with the most coverage and access as possible without breaking the bank? I have said it before and will say it again: we cannot provide everything for everyone for free. It’s a great idea, but it is simply not possible.